Broken hearts may be repaired
Prof. Michael Schneider is a leading authority in the field of cardiac molecular biology. In 2008, he obtained an ERC grant to identify the mechanisms governing self-renewal of cardiac progenitor cells, a population of stem cells located in the heart itself that might be exploited to play a key role in regenerating this vulnerable organ in heart disease. With his team at Imperial College London, he has now identified a stem cell injection that could mend broken hearts, a discovery in the field of regenerative medicine published this week in Nature Communications.
Written in collaboration the British Heart Foundation
During a heart attack, the heart is starved of oxygen and suffers damage that can never be repaired. When the heart is damaged, it becomes weak and cannot pump the blood properly. Over time, this damage can lead to heart failure, a condition that can only be cured with a heart transplant.
Over the last decade, stem cells isolated from the heart have demonstrated potential for encouraging the heart to repair itself – so called regenerative medicine. But there has been uncertainty within the research community around the best type and combination of stem cells.
In the research published in Nature Communications, a team from Imperial College London led by ERC grantee Prof. Michael Schneider and Dr .Michela Noseda has discovered a particular type of stem cell that could have the most potential yet for repairing irreversible damage caused by a heart attack.
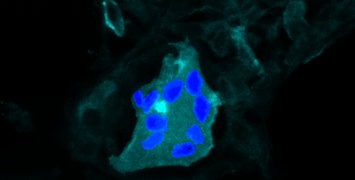
“We have found stem cells in the heart that have a specific protein – called PDGFRα – on their surface and had the greatest potential to repair damaged hearts," says Prof. Michael Schneider.
Stem cells that can transform into heart cells
Stem cells have the capacity to turn into any and all sorts of body cells, making a stem cell approach logical in order to repair heart muscle. Even though the adult heart in mammals cannot repair itself well after injury, Prof. Schneider’s research shows a new type of cell within the heart that can create new heart muscle in mice. The finding reveals that mice treated with these stem cells were able to recover and repair a significant proportion of their damaged heart muscle after 12 weeks, preventing heart failure, when compared to mice who had not received the stem cell treatment. The team used protein PDGFRα to find, purify and multiply enough of these stem cells, so that they could be injected into the damaged hearts.
“Now that we know which stem cells to use, we want to find their equivalent in human hearts for more efficient heart repair and regeneration after heart attacks," explains Prof. Schneider.
Heart-related diseases are the leading global cause of death. 17.3 million people die each year from cardiovascular illness and it is expected that this figure will grow to more than 23.6 million by 2030. The discovery is an early but important step towards heart regeneration, as it could lead to future treatments, like stem cell injections or use of the healing proteins that these cells make.
In 2007, Prof. Michael Schneider moved from Houston, USA, to London, as Head of Cardiovascular Science at the National Heart and Lunge Institute, Imperial College London. In the UK, he heads today the Cardiac Myogenesis, Death and Regeneration research group.
“My ERC Advanced Grant was indispensable to making a successful scientific transition from the US to the EU. Many of the innovative methods used in our new report were developed and perfected under the auspices of ERC support", stresses Prof. Schneider.
Scientific publication
PDGFRα demarcates the cardiogenic clonogenic Sca-1+ stem cell in adult murine myocardium.
Noseda et al. - Nature Comms, 18 April 2015
Portrait: ©Academy of Medical Science