Repairing the brain after a stroke

By Rosaria Carbone
A stroke occurs when an artery supplying blood to the brain becomes blocked, cutting off blood flow and causing damage to the brain tissue. Rapid intervention to remove the vascular occlusion in the acute phase is crucial.
However, beyond rehabilitative training, there are currently no specific treatments to promote recovery afterwards, as the mechanisms of brain regeneration remain poorly understood. While some patients regain, at least partially, some functions in the weeks or months following a stroke, almost 80% suffer from long-term impairment.
In the EU, an estimated 7.7 million people live with disabilities resulting from stroke and traumatic brain injury, placing a significant medical and economic burden on society. As a result, novel therapies to restore physical capacities after brain injury are urgently needed.
Investigating the immune system response
‘Acute brain injuries were once not considered neuroinflammatory disorders, but over the past decade, chronic brain inflammation has become a major focus of stroke research’, says Arthur Liesz.
‘The brain has been regarded as an immune-privileged organ, with no active immune system under normal conditions. However, after an injury, the immune system reacts very strongly, triggering a complex response that can either hinder or support the brain’s healing process.’
Recent research has revealed that T cells, a specific subset of immune cells, play a critical role in this response. Following brain injury, T cells invade the brain from the bloodstream. ’Although they are present in small numbers, T cells are extremely potent and behave in a seemingly contrasting way: in the acute phase, they trigger inflammation, exacerbating brain tissue damage. Surprisingly, during the chronic phase, they contribute to neurological recovery by supporting the growth of neurons and brain plasticity. The fundamental question is how T cells switch functions over time, and why. Understanding these mechanisms could unlock their therapeutic potential, allowing us to harness these cells as pro-regenerative factors,’ says Liesz.
The role of gut microbiota
The gut microbiome has a fundamental role in shaping the reactivity of the immune system. Changes in the microbiome composition can impact the immune functions, ultimately influencing inflammatory responses in organs affected by an injury, such as the brain following a stroke.
Given that the gut is the largest reservoir of T cells, Liesz hypothesized in his ERC-funded project RecoverInFlame that modifying the microbiome composition could provide a novel and safe way of shifting the immune response after stroke towards a pro-regenerative function.
During the project, Liesz’s team studied a specific group of bacterial metabolites called short-chain fatty acids (SCFAs). These are produced by intestinal bacterial fermentation and play a key role in activating the immune response. SCFAs induce the migration of T cells toward cerebral tissue. Since SCFA levels drop after a stroke, the team tested probiotic supplementation in animals, finding it beneficial for immune regulation and stroke recovery. Encouraged by these results, they conducted a clinical trial in stroke patients, administering them probiotics to restore gut microbiota composition and increase SCFA production.
‘We have concluded our first clinical trial and observed that probiotic treatment increased short-chain fatty acids and improved clinical outcomes. However, larger trials are needed for confirmation’ says Liesz.
Long-term inflammation
While a stroke’s immediate impact is well-known, its long-lasting effects on the body can be surprising. Inflammation occurs in all stroke patients, much like it does following an injury to any organ. However, while inflammation from a skin injury, for example, resolves quickly, brain inflammation does not decrease as easily – it can linger for a lifetime.
’What we discovered is that a stroke not only causes inflammation in the brain, but also leads to long-term changes in the balance of the entire immune system. Years after a stroke, a patient’s immune system remains altered, impacting not only the brain but also other organs, such as the heart,’ says Liesz. ‘This was actually surprising, as it emerged unexpectedly from our research, and we are now investigating it further. I think this is really a strength of ERC funding – it allows for the flexibility to conduct high-risk research, which leads to novel concepts and discoveries that you cannot achieve with strictly pre-planned studies.’
A multidisciplinary, innovative approach
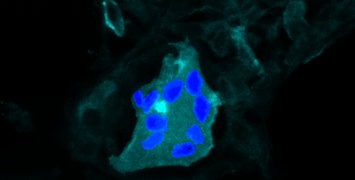
The complexity of this research necessitates a multidisciplinary team of bioinformaticians, imaging experts, neurologists and immunologists that combine expertise in various fields. The team also employed several innovative methodologies that have not been previously used in stroke research or neuroscience. For example, to better understand the movement of immune cells between organs, they use advanced tracking and labelling techniques in live mouse.
Liesz has also applied his therapeutic approach for stroke treatment in a mouse model of Alzheimer’s disease, observing that immune cells originating from the gut microbiome have also a significant impact on disease progression. By deepening our understanding of the interactions between the brain, the immune system, and gut microbiota, Liesz is paving the way for a new era in brain regeneration.
Biography
Arthur Liesz is Professor of Experimental Neurology at Ludwig Maximilian University Munich and board-certified neurologist at the University Medical Center. His research interest is on immunological aspects of acute brain injury, working on brain-immune interaction after acute brain injuries for nearly two decades. He is currently heading the Laboratory for Stroke-Immunology at the Institute for Stroke and Dementia Research, which spans across experimental studies using innovative preclinical research models as well as performing clinical studies including first-in-patient validation. He is principal investigator of the Excellence Cluster for Systems Neurology, recipient of several research awards and is coordinator of the German Stroke-Immunology network.