The shadow side of cancer treatment

More children than ever survive cancer now due to major leaps forward in treatments used to save these young lives. Overall, around 80% of children recover. The survival rate for Acute Lymphoblastic Leukemia (ALL), the most common childhood cancer, has risen to above 90%, while in the 1960s survival chances were practically nil.
“We are able to cure nearly every child, almost 97%, diagnosed with Hodgkin Lymphoma”, says Ruben van Boxtel. “In comparison, the survival rate for adults with this condition is only 50%. This difference exists because children can tolerate higher doses of chemotherapy, whereas adult patients would not survive such intense treatment.
After-effects
The use of high-dose chemotherapy in the treatment of childhood cancer, although successful in defeating the disease, often results, however, in long-term health problems for survivors. The after-effects include organ dysfunction, heart problems, fertility issues and an increased risk of secondary cancers. Although relatively rare, these new cancers present a significant challenge, as they are often difficult to treat.
Ruben van Boxtel and his team are specifically studying secondary leukaemia to understand how treatment of the original cancer can lead to this disease. His institute - the Princess Máxima Center for Pediatric Oncology– combines treatment and research in one facility, providing a centralized approach to childhood cancer care in the Netherlands.
Patients and their families are actively involved in the research process, while the centre’s scientists have access to the biobank, where bone marrow and blood samples as well as tissue biopsies of patients are stored for research purposes with their permission.
“The quick onset of secondary leukaemia in children, within 2 to 10 years of curing the first cancer, makes this disease an imperative case study”, says Van Boxtel. “These children are still minors when they return to our centre. Over the years, blood samples are taken for diagnostic purposes during different stages of treatment – during the first cancer, after the first cancer and during the second cancer. With these samples, we can study the development of the secondary leukaemia through time.”
Unique barcodes
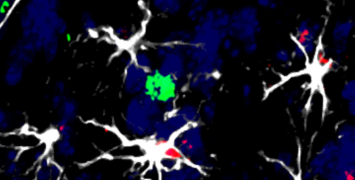
In order to trace back the origins of the secondary leukaemia, Van Boxtel and his team make use of DNA sequencing. All cells in the body have a unique repertoire of mutations, which are changes in the DNA code”, Van Boxtel explains. “As cells divide, they accumulate mutations, and as we age, our cells will have more and more mutations. Typically, most of these mutations are harmless passenger; mutations."
"We use these passenger mutations as unique barcodes to trace the origin of cancer. By creating a family tree of a patients blood cells, we can determine which branch of the tree gave rise to the leukaemia. This allows us to study the diseases development at various time points and extract patterns. By analysing the specific patterns or DNA scars' left by the mutations, we can deduce what processes caused the mutations. For instance, sunlight damages DNA differently than tobacco smoke, resulting in different types of mutations or scars in the DNA code. The same counts for chemotherapeutics.”
Clock-like signature
Van Boxtel explains that cancer treatments often includes a combination of different chemotherapy drugs, including platinum-based drugs that are also used in adult patients and thiopurines which damage replicating cells. It is known that these drugs cause a high number of mutations. Such mutations can become the drivers of the secondary cancer.
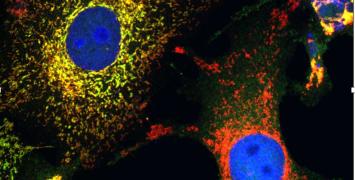
“Some mutational processes cause clock-like signatures, which are found in all tissues and can be compared with counting the rings of a chopped tree to determine its age”, Van Boxtel clarifies. “By sequencing normal stem cells, we can accurately estimate the age of the cell based on the presence of these mutations that accumulate in a clock-like manner over time.”
“We have found that children who have survived cancer have a higher number of these clock-like mutations compared to normal cells of the same age, indicating that they are molecularly older than they should be. This supports the idea that premature aging plays a role in the health problems they get after cancer treatment.”
Super stem cells
Although the underlying mechanisms are still being investigated, Van Boxtel and his team have noted that the mutation load goes up during treatment, but then normalises again after about 10 years. “The data we have so far are still suggestive, but it seems that the longer ago the cell experienced chemotherapy, the more the mutation load is going back to normal.”
“While mutations do not disappear and remain permanent, certain cells in the body seem to be better protected and able to withstand the effects of chemotherapy over time, these cells become more dominant, leading to a reduction in the mutation load observed in the samples. Are there ‘super stem cells’ that are protective and eventually reconstruct the tissue? If these exists it could have immense benefits for the treatment of children with blood cancer.”
Antiviral drugs
Not only chemotherapeutics but also certain antiviral drugs appear to cause secondary cancers. “When you are immune compromised, some viruses that we carry in our body can become overactive”, says Van Boxtel. “Normally, you won’t get sick, but if you don’t have an immune system, this can be very dangerous, so you have to take antiviral drugs. We found that some patients who had stem cell transplantation as a treatment had very high mutation loads. We figured out that a certain antiviral drug, ganciclovir, caused this.”
“For me, this was the most surprising finding of the last two years”, Van Boxtel continues. “This drug is still given to millions of people worldwide. Not only to children with cancer but also to people who need an organ transplantation.“
Replacing the more damaging antiviral drugs with safer alternatives seems quite easy because there are many substitutes available, according to Van Boxtel. “In contrast, replacing certain chemotherapy drugs is more difficult because they are so effective against the cancer. A challenge in childhood cancer treatment is that many children receive excessive doses of chemotherapy. How can we turn that around and start a clinical trial that aims to reduce the dose of chemotherapy? This is complicated and requires the careful identification of children who can receive lower doses to minimize the damaging side effects while still effectively treating the cancer.”
Biography
Ruben van Boxtel is a group leader at the Princess Máxima Center in the Netherlands. He obtained his PhD in rat genetics and studied the genetic stability of stem cells in human organoid cultures. He later moved to characterize how stem cells accumulate mutations throughout life and how this contributes to carcinogenesis. He has received prestigious awards such as the NYSCF Robertson Stem Cell Investigator award in 2022 and was selected as an Oncode Investigator in 2019 for innovative cancer research.